Retailers know they have to find the right blend of digital convenience and in-person service. Consider Walmart’s latest advertising campaign in which customers gleefully place orders online and through its app, selecting to receive smart-looking blue boxes on their doorsteps or seamlessly pick up their orders at the closest store.
Imagining the same ad for a healthcare provider in 2018, even an innovative provider, is a stretch.
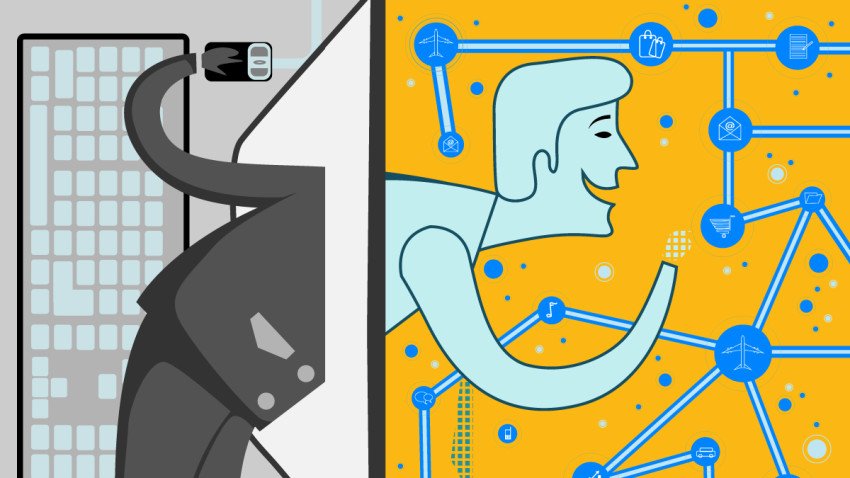
Like banks, airlines, and retailers, health care providers will need to offer an easy, digital front-end experience to their customers. This isn’t just about building fancy new websites, but undertaking true care redesign: becoming adept at delivering high-quality, cost-effective virtual care through telehealth and digital tools. To this end, they will need to move from pilot programs to large-scale efforts routinely offered across the care spectrum.
The challenge is huge. It requires a business designed entirely around in-person interactions and in-house procedures, staffed by professionals who trained and likely practiced for years in these settings and no others, currently operating at or beyond maximum capacity, to now accommodate customers through diametrically opposed processes: Caring for patients who are not physically present, using processes in which the clinicians have little formal training, imperfect tools, and only preliminary data. To survive this evolution, provider organizations need to ask three key questions.
First, what strategic goal would virtual care help achieve today? For some providers, virtual care is about meeting a perceived and growing consumer need: this is what my patients want and will increasingly expect. Indeed, among its clearest benefits is patient convenience. For providers measuring patient experience precisely enough, virtual care may improve these scores (indeed, among Brigham and Women’s Hospital patients surveyed after their initial telehealth encounter, 97% were satisfied with the experience and would recommend the program, and 74% felt that the interaction actually improved their relationship with their provider). Improved access is another potential benefit, as telehealth tools can free up time for providers to see new and more complex patients in-person by efficiently moving more routine visits out of the office. For health care systems engaged in risk contracting and alternative payment models where there are penalties for increasing total medical spending too quickly, telemedicine can help improve contract performance by reducing utilization of the services and clinical events that are driving expenses.
These are all very different strategic needs requiring different implementation approaches and performance metrics. The second question providers must ask is how they will measure the success of their virtual care services. If they’re not already, academic medical centers and providers who can partner with one should conduct randomized trials of their efforts and publish the results. Without better data, we will know little about the true effectiveness of virtual health care technologies. When formal research trials aren’t practical, providers will need to embrace A/B testing and learn to more rapidly evaluate the effectiveness and scalability of these technologies. At Brigham Health, we are testing the use of virtual outpatient visits in a large randomized trial this year and measuring outcomes. In another randomized study conducted by Brigham Health and Massachusetts General Hospital we are looking at whether virtual health coaching and communicating with patients by text can improve blood pressure across a large population. These data will be critical for scaling: it can be difficult to convince clinicians to see patients virtually, or to offer their patients digital health tools, without compelling evidence of real benefit.
Even with persuasive evidence for implementation, the third question for providers, already stretched thin by clinical and other work responsibilities, is how will they the find the time and resources to experiment with the growing list of digital tools? Over the past year I’ve watched hundreds of physicians, nurses, nutritionists, pharmacists and other providers across Brigham Health practices start offering virtual care tools in dozens of ways, from specialist virtual visits, to primary care digital questionnaire-based encounters, to routine remote measurement of patients’ clinical data from home, along with other of digital health interventions such as smartphone apps. These clinicians are making it work, but it is challenging: to many, it feels like a new job.
Traditional provider organizations need to find ways to offer these services not just at the margins of the day, and not just by small pockets of early adopters. There are solutions to this problem, but they require material restructuring and can be costly. One approach is to include non-physician providers in staffing telemedicine programs; we are experimenting with having licensed providers of all kinds including physician assistants, nurses, and nutritionists deliver virtual care. Physicians can dedicate more of their schedules to virtual care, but will need more flexible hours and appropriate compensation to accommodate this shift. Practices will need resources as they would for any large rollout — think of the resourcing of the national Patient-Centered Medical Home movement, but applied to comprehensive digital care. And finally clinicians will need careful education and training for digital health, which is by and large not found in national training and continuing education programs.
There are other structural barriers providers will need to overcome in a hurry. One is provider licensing, a critical limiter of regional and national market share. Care systems are either entirely or predominantly licensed only in a single state, whereas dedicated digital care companies will establish licensure in all fifty. Another is technology: Like Walmart, providers will need to integrate a digital platform into their existing model. Until EMR vendors offer great digital health tools as part of their standard systems, we will need to design or license these ourselves. As Fast Health Interoperability Resources (FHIR) and Meaningful Use Stage 3 create more connections between electronic records, patient data, and personal health apps, the technology landscape will begin to change very quickly in 2018, with digital care delivery front and center.
Healthcare providers, like retailers and other traditionally in-person businesses, need to prepare for a future where technology companies, focused solely on delivering care virtually, increasingly meet the needs of patients more conveniently and efficiently. Providers can either cede market share and volume to these companies, or beat them at their own game by scaling their own virtual care services. Strategic decisions providers make today will determine how ready they will be for a future where patients expect their healthcare to be as seamless as online shopping, if they are to remain loyal.
[“Source-hbr”]